(This is the second of 2 posts about a possible link between intestinal bacteria, obesity, and other chronic illnesses.)
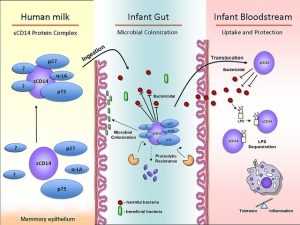
The most enlightening article I’ve seen about micrbiota (gut bacteria) research is an April 2013 article from Mother Jones. It explores the possibility that insulin resistance (see previous post) is actually an “inflammatory” process caused by the production of “endotoxin” by unhealthy gut bacteria.
The Major Health Implications of Dysbiosis
Owing to a doubling of obesity rates since 1980, this strikes me as a reasonable hypothesis. The mass marketing of antibiotics by Big Pharma, Food Inc (in livestock feed), and Monsanto (in genetically modified organisms) has led to epidemic levels of dysbiosis (a derangement in gut bacteria) in the industrialized world. In addition to skyrocketing obesity rates, the developed world has also experienced a significant increase in other dysbiosis-related conditions, including cancer, diabetes, and degenerative and autoimmune disease. It would also explain why children born to obese mothers (we acquire gut bacteria from our mothers) are more likely to suffer from asthma, attention deficit disorder, and autism.
The article cites research from the University of Washington showing that foods high in saturated fats and sugar promote the growth of endotoxin-producing inflammatory bacteria. Endotoxin, in turn, causes inflammatory damage to the the hypothalamus, the brain’s appetite center. When this occurs, people lose the ability to feel full and eat to excess.
The Mother Jones article also references studies in which volunteers improved their insulin sensitivity, as well as losing weight, by reducing their level of “inflammatory” bacteria. They accomplished this by consuming diets rich in fermented foods containing healthy, anti-inflammatory bacteria.
Most interesting of all are studies showing that bariatric (weight loss) surgery helps some patients and not others depending on their ability to grow a healthier microbiota (gut bacteria colony) following their procedure.
The Care and Feeding of Intestinal Bacteria
After suffering a sudden onset of so-called “irritable bowel” syndrome 20 years ago, I have a strong personal interest in dysbiosis. The Sydney GI specialist I consulted says the only effective treatment for most IBS sufferers is to re-establish a healthy microbiota.
The end of the article offers a number of suggestions how to accomplish this. The bottom line is to consume a diet rich in 1) fermented foods with live bacterial cultures and 2) complex carbohydrate and fiber-rich foods these organisms thrive on. Studies show that treatment with whole foods is always preferable to taking probiotics. Fermented foods contain literally thousands of strains of bacteria that work collaboratively with one another. Probiotic capsules, in contrast, contain a dozen strains at most and are likely to be destroyed by stomach acid
Examples of helpful fermented foods include sauerkraut (only if it’s made via fermentation), miso (fermented soybean paste), kefir (a fermented drink), and some yoghurts. To ensure the bacterial cultures are live, it’s best to ferment these foods yourself or get them from a reliable health food store. It’s also essential to check the label to make sure they aren’t pasteurized (pasteurization kills bacteria).
The foods these bacteria like to munch on include onions, garlic, potatoes, bananas, yams, apples, oranges, whole grains, Jerusalem artichokes, legumes and cruciferous vegetables (cabbage, broccoli, and cauliflower).
Looking after the new bacteria in my intestine is almost like having a new pet to care for. I can already tell from my symptoms which foods they really like: yam, cooked apples, and avocado. Luckily I’m pretty keen on them myself.
photo credit: www.cihr-irsc.gc.ca via photopin cc

Pingback: The Taboo Against Animal Fat | The Most Revolutionary Act
Reblogged this on PliscaPlace.
LikeLike